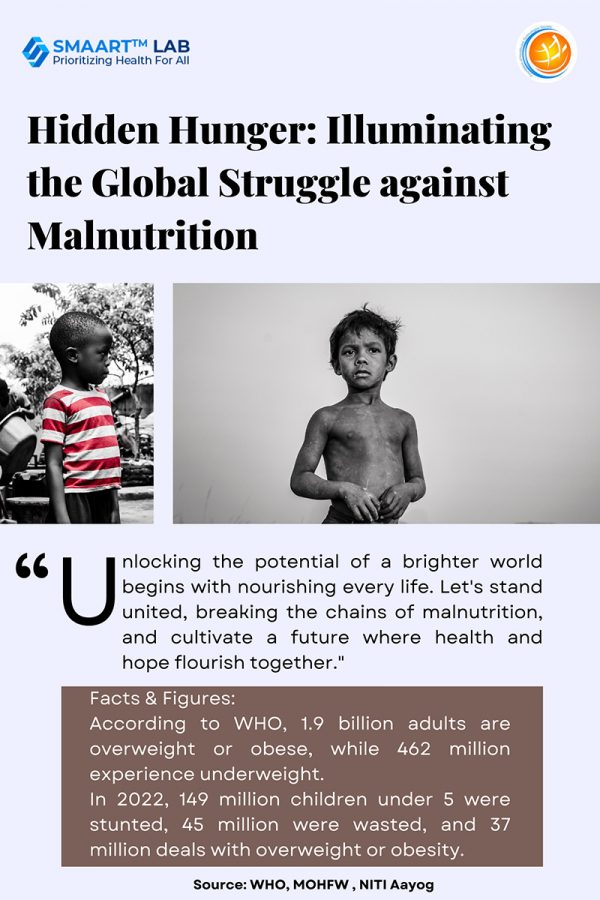
Malnutrition is a global health crisis affecting billions of people. According to the World Health Organization, In 2019, 1.9 billion adults grappled with being overweight or obese, while 462 million were underweight. In 2022, 149 million children under 5 were identified as stunted, 45 million as wasted, and 37 million dealing with overweight or obesity.
According to the National Family Health Survey of India (NFHS-5, 2019-21), stunting (35.5%), underweight (32.1%), wasting (19.3%), and severe wasting (7.7%) prevail among children under 5. Despite a decline in under nutrition, progress seems slow in India.
Understanding Malnutrition
Malnutrition encompasses deficiencies or excess in nutrient consumption, an imbalance of crucial nutrients, or hindered nutrient utilization. The dual burden of malnutrition involves both under nutrition and issues related to excessive weight, such as overweight and obesity.
- Wasting is an acute malnutrition characterized by insufficient weight relative to height, stemming from an inability to gain weight or actual weight reduction.
- Stunting is characterized by insufficient height relative to age, indicating a failure to attain the expected height/length compared to a healthy, well-nourished child of the same age.
- Underweight is defined as insufficient weight relative to age. A child classified as underweight may experience stunting, wasting, or a combination of both conditions.
- Micronutrient deficiencies refer to an insufficiency of important vitamins and minerals necessary for bodily functions.
- Overweight and obesity occur when an individual exceeds a suitable weight for their height. The accumulation of abnormal or excessive fat can negatively impact health.
Acute malnutrition can be categorized into two groups: Moderate Acute Malnutrition (MAM) and Severe Acute Malnutrition (SAM). Moderate Acute Malnutrition (MAM) is characterized by moderate wasting, while Severe Acute Malnutrition (SAM) occurs when a child experiences severe wasting, with or without accompanying body swelling due to fluid retention.
Causes of Malnutrition
Malnutrition can occur due to various factors, including low family income, extensive family size, gender bias, diminished absorption of macro- and/or micronutrients, increased losses or altered requirements, heightened energy expenditure (especially in specific disease processes), changing crop patterns resulting in reduced dietary intake, loss of traditional food habits, lack of access to food, and insufficient knowledge.
Approaches to address malnutrition in children
The Government tackles under nutrition through initiatives like POSHAN Abhiyaan, focusing on a life-cycle approach. Schemes like Anganwadi Services and Pradhan Mantri Matru Vandana Yojana (PMMVY) address nutritional needs of adolescents, pregnant/lactating women, and children. Mission Poshan 2.0 enhances efforts, emphasizing maternal nutrition, child feeding, and AYUSH wellness. It promotes diet diversity, food fortification, and millet use to combat deficiencies. Millets, rich in nutrients, feature prominently in hot meals and take-home rations. Poshan Vatikas nationwide offers affordable access to fruits, vegetables, and medicinal plants, creating a holistic approach to break the cycle of malnutrition.
Guidelines for Evaluating and Addressing Malnutrition in Children
The procedure for evaluating and addressing malnutrition in children comprises multiple stages. Initially, growth monitoring through anthropometric measurements is employed to identify malnourished children. Severe cases undergo active screening for edema and wasting. Subsequently, an appetite test is administered for children with severe acute malnutrition (SAM). A medical assessment follows, determining the level of care based on the extent of malnourishment. Nutritional management, with specific meal plans tailored to age groups is implemented across different care levels.
| Age | Type of Meal | Energy(Kcal) | Protein (g) | Total Fat (g) | Carbohydrate (g) | Cereal: Pulse Ratio | Calcium (mg) | Zinc (mg) | Iron (mg) | Folate (µg) | Vitamin A (µg) | Vitamin B6 (µg) | Vitamin B12 (µg) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Undernourished Children (6-12 months) | Take Home Ration | 400 | 15-20 | 15-18 | 35 | 2:1 | 200 | 1.5 | 1.5 | 50 | 115 | 0.35 | 0.66 |
| Undernourished Children (1-3 years) | Take Home Ration | 700 | 25-30 | 25-30 | 70 | 2:1 | 270 | 2 | 4 | 70 | 120 | 0.55 | 0.66 |
| Undernourished Children (3-6 years) | Morning Snack + Hot Cooked Meal + Take Home Ration | 800 | 25-30 | 25-30 | 70 | 2:1 | 300 | 3 | 6 | 80 | 160 | 0.66 | 1.24 |
Children with SAM receive additional nutritional allowances (If the child is supposed to receive the entire day’s food from Anganwadi Center, the child should be provided energy @120kcal/kg body weight/day). Medical management is administered as required. Education on nutrition, hygiene, and follow-up care is emphasized. The protocol includes ongoing monitoring and referral processes to ensure the well-being of malnourished children.
Call for Action
In 2015, the world pledged to achieve the Sustainable Development Goals (SDGs), targeting the eradication of malnutrition by 2030. Despite these commitments, around 45 million children under five suffered from acute malnutrition globally in 2022. Approximately 7.3 million children received severe acute malnutrition (SAM) treatment in 2022. Despite increased treatment coverage, many affected countries still struggle to provide necessary care for children with SAM.
The Global Action Plan (GAP) on child wasting recognized the necessity for updated guidance. WHO responded by creating a comprehensive guideline with evidence-based recommendations. Key guideline recommendations include a child-centered approach, caring for mothers and infants as an interdependent pair, promoting breastfeeding, encouraging access to nutrient-dense home diets for prevention and management, and acknowledging the crucial role of community health workers in delivering evidence-based care for children with acute malnutrition. WHO collaborates with UNICEF and other UN agencies to develop practical operational guidance, aiding policy-makers, program managers, and health workers in implementing the guidelines.
References
- https://www.niti.gov.in/sites/default/files/2023-12/CMAM-report-NITI-Aayog.pdf
- https://www.who.int/health-topics/malnutrition#tab=tab_1
- https://wcd.nic.in/sites/default/files/CMAM-Book-10-10-2023%20%281%29.pdf
- https://www.who.int/news-room/fact-sheets/detail/malnutrition
- https://www.who.int/news/item/20-11-2023-who-issues-new-guideline-to-tackle-acute-malnutrition-in-children-under-five
Authors
Janhvi Sahai 1
- Janhvi Sahai, v-INSPIRE Intern